Wear and tear arthritis or Osteoarthritis (OA) is the most common type of arthritis. It happens when the rubbery lubricant material between the bones, called cartilage, breaks down. This leads to joint damage from bone rubbing on bone.
Though the elderly are more commonly affected, arthritis can in occur in the young and middle-aged as well. Being a degenerative disease, OA generally worsens over time.
As cartilage wears, joint surfaces become pitted and rough – causing pain and irritation within the joint and in surrounding tissues. Cartilage is avascular and cannot repair itself. The breakdown of cartilage also brings the bone surfaces closer together, which leads to the growth of bone spurs (or osteophytes). Bone spurs are sharp, hard bumps of extra bone that form along the periphery joints as a result of joint injury. The spurs themselves are painless, but can cause stiffness in the affected joint. Bone spurs are an indication of OA.
There are 4 stages of OA. These are graded on the basis of X-ray findings and help gauge the need for surgery.
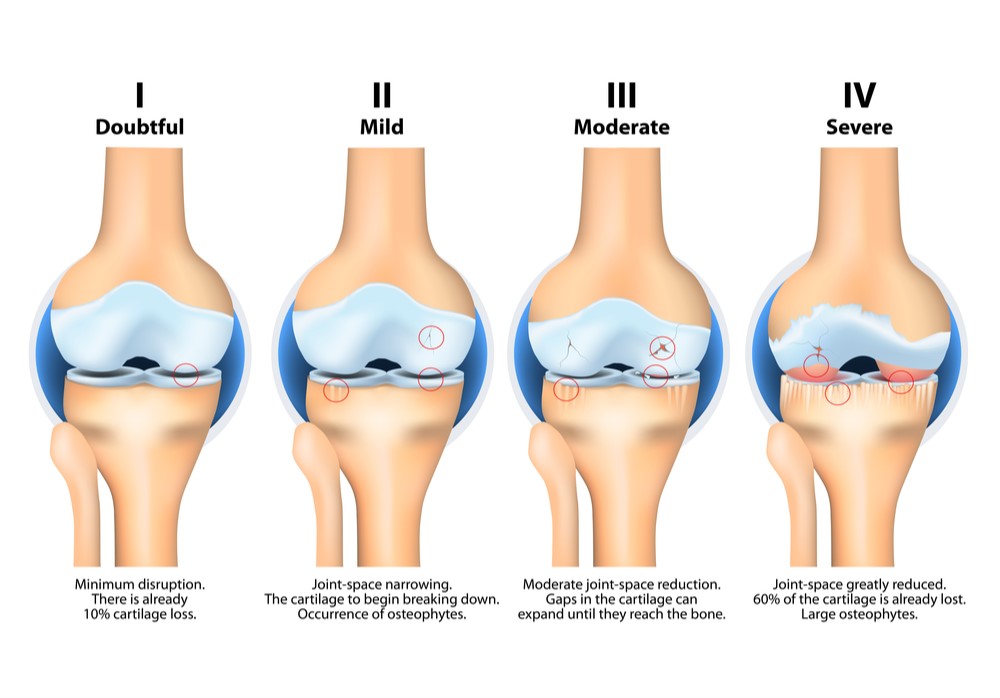
The symptoms of each grade vary from person to person. Some individuals experience few symptoms despite joint deterioration, while some experience significant pain and stiffness that affect their daily activities.
Unfortunately, there is still no way to reverse established OA. Anti-inflammatory and pain medications are often prescribed to ease the discomfort caused by the onset of OA. These medications help patients cope with their pain and carry on with their daily lives, but do not cure the underlying condition. Likewise, physiotherapy can help reduce the pain and stiffness in early and moderate OA, but cannot repair the underlying joint damage. Hence, as the OA increases in severity, surgical intervention may become the only remaining effective treatment option.
Osteoarthritis can be classified into Primary OA and Secondary OA.
Primary OA is generally age-related. As joints age, the water content of cartilage increases while the collagen and other proteins that make up cartilage are broken down. Constant use of the joints over time causes further damage to the cartilage.
Bone remodelling occurs over time in the degenerative joint, leading to the formation of spurs and bone cysts. In severe cases, complete degeneration of cartilage causes friction between the bones, leading to worsening pain and stiffness.
Secondary OA is related to injury or other diseases, such as obesity. Other causes could include trauma, post-surgical complications, congenital abnormalities, hormonal disorders, gout, rheumatoid arthritis, and other inflammatory disorders.

There are some preventive measures one can take to slow down the development of Primary OA and delay the onset of Secondary OA. These include:
- Keeping a healthy body weight – Excess weight increases the stress on the joints and extra fat speeds up changes in the cartilage complex.
- Control your blood sugar – Diabetic patients have a higher risk of getting OA. Diabetes can affect the musculoskeletal system, causing joint and nerve damage.
- Lead an active lifestyle – Leading a sedentary lifestyle can make joints stiff and speed up muscle degeneration. This adds to the stress placed on the joints leading to a quicker onset of OA.
- Prevent joint injuries – Stretching and warming up before exercise can help your muscles and joints get ready for excessive use. People recovering from previous injuries and/or haven’t exercised in a while should use protective gear as a form of joint support.
- Listen to your body – Pain is the natural protective indicator of the body when it’s under excessive stress. Rest and moderation in exercise can lead to a lower incidence rate of injury.
Oral supplements such as collagen, glucosamine and chondroitin can also reduce the symptoms of OA.
Onset of osteoarthritis is generally gradual, usually localised to a single joint in the beginning. Deep aching joint pain is commonly the first symptom. As OA progresses, joint motion can become restricted and tenderness, along with cracking sounds and grating sensations, can be felt. Some other symptoms are:
- Pain that may worsen at the end of the day or when moved
- Stiff joints that feel better after moving
- Swollen joints
- Muscle weakness around the joint
- Joint instability or buckling
- Noticeable deformities (e.g. bow-leggedness, knock-knees, slanted heels with abnormal shoe wear)
Non-modifiable risk factors (factors you cannot change):
Age: As you grow older, your risk of OA increases.
Gender: According to the National Institutes of Health, OA is slightly more prevalent in men until the age of 45. After that, it appears more common in women.
Modifiable risk factors (factors within your control):
Previous Injury: People who have injured a joint are more likely to develop OA in that joint.
Poor Posture: Sitting or standing in a poor posture can cause extra strain on the joints to compensate for the body’s altered centre of gravity.
Diabetes: Patients with type 2 diabetes have an increased risk of OA. Overconsuming processed sugar also causes the body to release cytokines which add to joint wear-and-tear.
Obesity: Obesity and excess body fat put increased mechanical stress and strain on the body – increasing the risk of OA in the joints.
Physical Inactivity: Being immobile for long periods of time can cause your joints to stiffen. This makes movement more likely to hurt. Inactivity during the night may partially explain why OA pain is often worse when on awakening in the morning.
Occupation-related: Repetitive actions can put undue stress on your joints. Some occupations that require lifting, climbing, walking, kneeling/ squatting for more than an hour a day may act to increase the risks of OA. Competitive sportsmen can also be more susceptible to OA.
Environmental Conditions: Cold weather and barometric pressure can cause joints to expand and the thickening of synovial fluid (the fluid within joints), leading to stiffer and more painful joints
Other Medical Conditions: Medical conditions that affect joint health can affect your risk for OA. For example, bleeding disorders can cause bleeding in the joints. Conditions that affect blood flow or inflammation can also affect risk. Some medical conditions associated with OA include:
- Osteonecrosis
- Paget’s disease of bone
- Diabetes
- Gout
- Underactive thyroid
Though many risk factors are secondary and changeable, osteoarthritis is fundamentally a degenerative disease. However, the more secondary risk factors you have, the higher risk you have of developing OA.
OA typically affects the spine and weight-bearing joints such as the knee, hip, ankle and foot joints. For this article, we will focus on the major weight-bearing lower limb joints.
Knee Osteoarthritis:
Background
The knee is the most commonly affected joint in the body. Knee OA mainly affects people over the age of 45. Knee OA can lead to pain and loss of function, but not everyone with radiographic findings of knee OA will be symptomatic.
Symptoms
Signs of knee OA are:
- Joint stiffness that may be worse in the morning
- Dull achy pain
- Pain after increased activity
- Limited range of movement (ROM)
- Pain after prolonged sitting or lying
- Pain on joint line palpitation
- Joint enlargement
- Difficulty weight bearing on the affected leg
- Decrease in abilities of daily functioning
- Sleep affected (severe)
Diagnosis
Knee OA is diagnosed via clinical examinations and confirmed by X-rays.

Diagnostic tests:
- Physical Examination
- Blood Tests – to help determine the type of arthritis
- Arthrocentesis – A sterile needle is used to take samples of joint fluid which can then be examined for signs for inflammation, infection or gout.
- Arthroscopy – A camera is inserted in the affected joint to obtain visual information about the damage caused to the joint by the OA and perform minor repairs if needed.
- MRI – Provides high-resolution images of cartilage, meniscal and ligamentous injuries, and other structural abnormalities typical of OA.
- X-rays – The most important initial imaging modality that provides information on the severity of OA, as well as the associated bone injuries and degree of joint deformity.
Treatment
Non-surgical
- Weight loss therapy
- Physiotherapy and knee bracing
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
- Intra-articular corticosteroid injections
- Intra-articular hyaluronic acid injections
- Other therapeutic Injections
Surgical
An array of surgical options are available for the effective treatment of knee arthritis, depending on the patient’s age, activity level, and severity of arthritis:
- Arthroscopy – Trim or repair degenerative meniscal tears and remove loose bodies
- High tibial osteotomy (HTO) – An option for very young and very active patients with localized arthritis
- Patellofemoral joint arthroplasty – For younger patients with isolated patellofemoral joint arthritis, with the rest of the knee (tibiofemoral compartments) being healthy
- Uni-compartmental/ Partial Knee Arthroplasty (UKA) – Probably the best option for both younger and older patients who suffer from arthritis in only one knee compartment (medial or lateral)
- Total knee replacement (TKR) – The mainstay treatment for advanced knee arthritis affecting more than one compartment of the joint
Hip Osteoarthritis
Background
Hip OA is one of the top contributors of global disability. It is prevalent in 10% of people above 65, and 50% of these cases are symptomatic. The most common symptom of hip OA is pain around the hip joint, which develops slowly and worsens over time.

Risk Factors
- Hip trauma (injury/fracture) – results in unilateral hip OA
- Inflammatory arthritis
- Congenital & developmental hip disease (e.g. Perthe’s disease, developmental hip dysplasia, etc.)
- Avascular necrosis (death of bone due to lack of blood supply caused by prior injury or fractures, medications such as steroids, alcohol, blood disorders, etc)
- Abnormal joint morphology (femoroacetabular impingement or FAI)
- Acromegaly and metabolic diseases
- Ethnicity (80-90% less prevalent in the Asian population)
Symptoms
Signs of hip OA are:
- Joint stiffness that may be worse in the morning
- “Locking” of hip movement
- Movement induced crepitus (abnormal popping or cracking sound)
- Limited range of movement (ROM)
- Leg length discrepancy
- Localised inflammation
- Gait abnormalities – short limb gait, antalgic gait, stiff hip gait, etc.
- Progressively increasing and easily aggravated pain
- Pain commonly in groin/thigh, radiating to buttocks or knee
Diagnostic Procedures
Hip OA is diagnosed via physical tests and confirmed with X-rays.

Diagnostic tests:
- Physical examination testing hip’s range of movement, swelling, muscle weakness and area of tenderness (usually groin)
- X-rays – The most important initial imaging modality that provides information on the severity of OA, as well as the associated bone injuries and degree of joint deformity.
- MRI – Provides imaging of the cartilage, tendons, soft tissues and bone of the hip; may be helpful in evaluating for other causes of hip pain
- Ultrasound – Evaluates soft tissue structures that surround the hip joint & identifies changes to joint lining and fluid volume
- CT Scan – Occasionally useful for assessing bone defects in severe OA
Treatment
Non-surgical
- Physiotherapy for muscle strengthening
- Modification of risk factors such as weight control, limiting high-impact activities and minimisation of pain aggravating activities
- Painkillers
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
- Intra-articular corticosteroid injections
- Intra-articular hyaluronic acid injections
- Other therapeutic Injections
Surgical
- Total hip replacement – the gold standard for severe hip OA
- Hip osteotomy (rare) – for very young patients with early localized OA

Background
Ankle OA is less prevalent than other forms of lower limn OA (hip and knee). This is due to the fact that there is relatively good stability in the ankle joint. Usually, the main cause of ankle arthritis is trauma, although secondary arthritis from other medical conditions can occur (e.g. gout, rheumatoid and other inflammatory diseases).
Symptoms
Some symptoms that may present with ankle OA are:
- Pain in the lower shin, ankle, heel or middle of the foot
- Stiffness of ankle
- Swelling
- Crepitus
- Instability of ankle (locking or buckling)
- Abnormal gait (e.g. limping)
Risk Factors
Ankle OA has similar risk factors as other forms of OA, including genetics, excess weight, trauma, age and physical inactivity. The main predisposing factors are previous ankle fractures or a history of recurrent sprains and ankle instability. Foot conditions such as flat foot (pes planus) and high-arched foot (pes cavus) can also lead to ankle arthritis in the latter stages.
Diagnosis
Diagnosis of ankle OA is via a physical examination and can be confirmed by radiological tests.
Diagnostic tests as similar to those described above for hip and knee OA:
- Physical examination
- Radiology
- X-rays
- MRI
- CT scan
- Lab tests
- Used to rule out other problems (such as rheumatoid arthritis)
- Involves blood tests and drawing fluid from the joint
Treatment
Non-surgical
- Physiotherapy
- Footwear modification and orthoses (e.g. corrective insoles)
- Support devices (e.g. joint braces, canes)
- NSAIDs & pain-relieving drugs
- Intra-articular corticosteroid injections
- Intra-articular hyaluronic acid injections
- Other therapeutic injections
Surgical
- Arthrodesis – Ankle fusion surgery reduces pain by eliminating motion in the ankle joint, and is conventionally performed through open surgery. Surgeons trained in minimally-invasive surgery (MIS) are able to perform this procedure through arthroscopic “keyhole” surgery, which allows for much less pain, faster recovery, better fusion rates, and lower complications compared to open surgery.
- Total Ankle Replacement (TAR): TAR is a state-of-the-art treatment that is particularly useful in patients who require preservation of their ankle movement, often due to work (e.g. truck drivers) or sporting activities (e.g. skiing, cycling, etc).
Just like any other joint in the body, the foot is also susceptible to arthritis and damage to the cartilage over many years of strain and trauma. If severe, it can greatly affect your quality of life and limit your ability to walk properly.
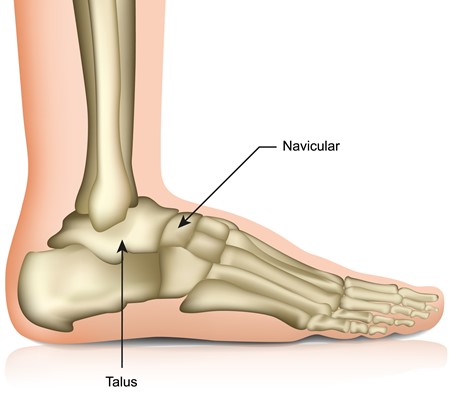
The talus is one of the important load-bearing foot bones and is involved in 2 important hind foot joints – 1) subtalar joint (the joint below the talus) is involved in the sideways tilting movement (inversion & eversion) of the foot; 2) talonavicular joint (the joint in front of the talus) is involved in complex tri-planar movements of the foot. Lastly, the calcaneocuboid joint lies adjacent to both the subtalar and talonavicular joints, and is also involved in tri-planar movements of the foot. One, two or all of these joints may be damaged and become arthritic in foot injuries and chronic conditions such as pes planus (flat foot) and pes cavus (high-arched foot).
In subtalar, talonavicular and/or calcaneocuboid fusion surgery (also called triple fusion or triple arthrodesis), the areas of damaged bone & cartilage in these joints are carefully removed. After restoring the correct shape of the foot, the subtalar, talonavicular and/or calcaneocuboid joints are held in place with metal screws or plates. Similar to ankle fusion (described above), the bones in these joints will fuse together, resulting in greater stability and reliable pain relief.
When done using the “keyhole” technique, arthroscopic triple fusion has much lower skin complications and infections that are problematic with open surgery. Arthroscopic triple arthrodesis has the additional benefits of much less pain, more rapid recovery, earlier discharge home (often within a day), and better fusion rates. Patients typically report better and faster return to activity and work following arthroscopic triple fusion.
Lastly, arthritis can also develop in the joints in the middle (midfoot) and front (forefoot) of the foot. These conditions can initially be treated with analgesics, footwear and activity modification. When severe, however, OA of the midfoot and forefoot can be effectively treated with surgical fusion of the affected joints, typically with excellent results.
Although OA cannot be reversed, the outlook is very positive with treatment. Chronic joint pain, stiffness and deformity should not be ignored, particularly in the weight-bearing joints of the lower limb that are crucial to your mobility and daily activities. Do seek early consultation with your doctor if you have any concerns. The sooner treatment is administered, the better the outcomes, and the sooner your quality of life can be improved.


